Emmanuel Hospice presented the Sister Gabriela Caring Spirit Award to Dr. John “Jack” Hartmann during a volunteer luncheon on Friday, Nov. 8 at Waterford Place in Jenison.
The award recognizes a volunteer who carries with them the mission and vision of Emmanuel Hospice and who goes above and beyond with their compassion for patients and their families. The award was named after Sister M. Gabriela Hilke, the founding visionary behind the creation of Emmanuel Hospice and the award’s first recipient. She is also a spiritual caregiver and active board member with the organization.
“Jack came to mind right away when our team was deliberating who should receive the award this year,” said Jackie Chandler, volunteer coordinator. “Jack has been incredibly engaged and passionate about Emmanuel Hospice from the very beginning. We have appreciated his continued dedication to our patients, and the many times he’s exceeded our volunteer expectations.”
A retired OB-GYN, Hartmann started volunteering with Emmanuel Hospice in the fall of 2018. He was first trained as patient/family support volunteer, helping to enhance patients’ quality of life through companionship, one-on-one time and prayer. When Emmanuel expressed a need for vigil volunteers, Hartmann was quick to sign up for the training.
Vigil volunteers must be compassionate listeners who recognize the transition that takes place at the end of life is both physical and spiritual. They are called on at all hours and any day of the week to be there for patients when no else can be to ensure no one dies alone. Vigil volunteers bring families some peace of mind knowing someone could be there with their loved one.
“Jack has been called to serve in this capacity multiple instances. Time and time again, no matter the hour, he’d be there – and he has sat bedside with patients for hours,” Chandler said. “I’ll never forget when I asked Jack why he was interested in volunteering, and he simply replied, ‘there is dignity in listening.’
“That really struck me. That’s exactly the mindset we look for in volunteers.”
Hartmann is also known for being an advocate for patients. He has developed meaningful and close relationships with the patients he has worked with, paying special attention to their needs. He has sought out trainings to learn how he can better support individuals with different conditions, such as those with dementia.
When he recognized one patient in particular was really struggling emotionally, Hartmann reached out to the interdisciplinary team to inquire about whether it would be OK for him to visit that patient more often than what is asked of volunteers. Emmanuel Hospice commended Hartman for his collaboration with the interdisciplinary team to ensure that patient received the additional support needed.
“People facing end-of-life issues experience some of the most important days of their lives,” Hartmann said. “For me, to be a possible source of kindness, even for a few hours, for such individuals is a privilege.
“I am very grateful for Emmanuel Hospice for giving me the opportunity to serve.”
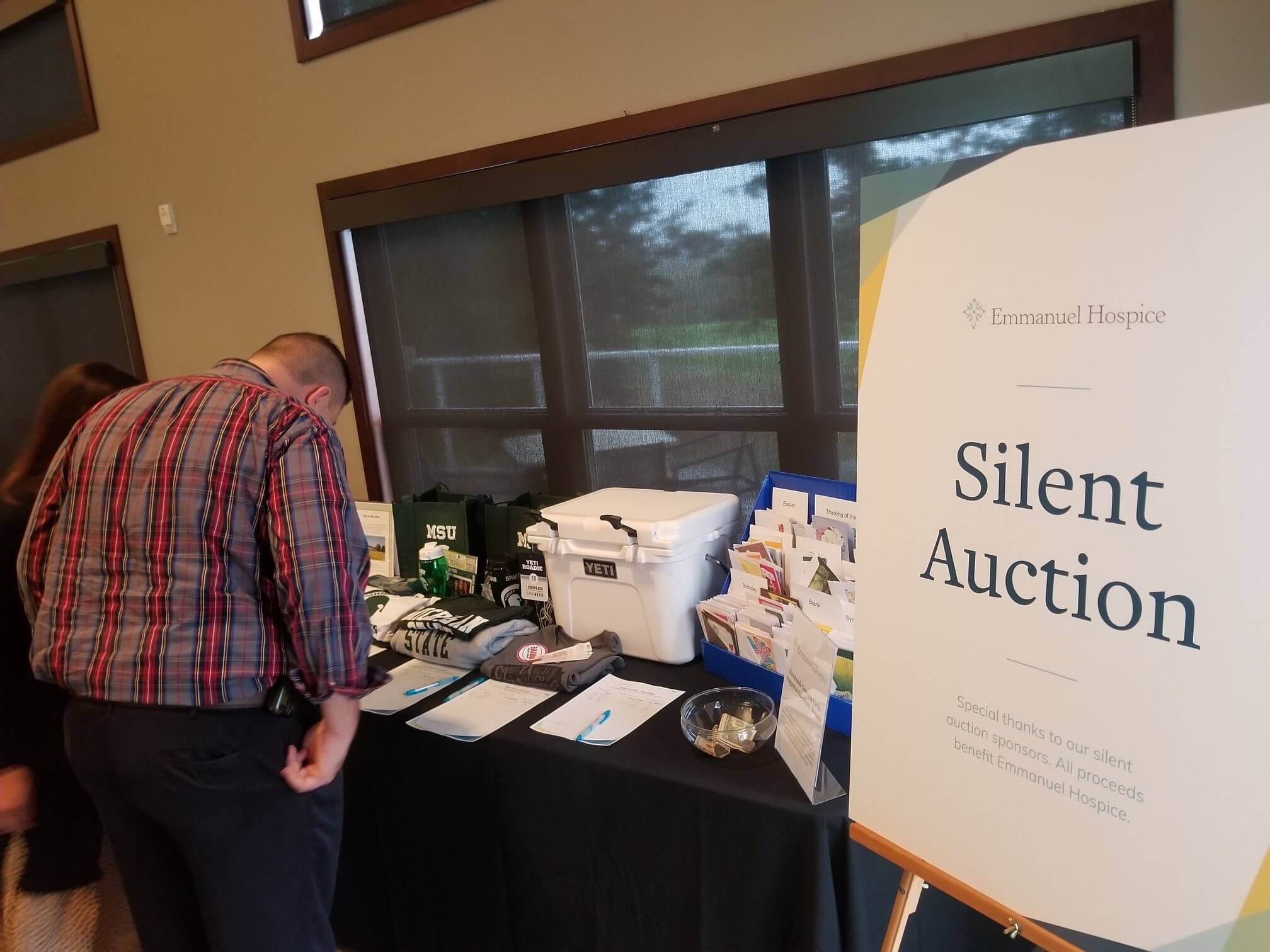
Volunteers serve Emmanuel Hospice in many ways, including making bereavement calls, capturing patient’s life stories, supporting office needs and providing companionship with certified pet visitors. Other volunteer opportunities include assisting with art therapy, community outreach, knitting, card-making and patient/family support. So far this year, 35 volunteers have donated more than 2,100 hours to the organization, a cost savings of more than $38,000.
Emmanuel Hospice currently has a need for patient/family support and pet visitor volunteers. Pet visitor volunteers are trained as patient/family support volunteers in addition to having their pet certified as a companion animal.
The organization is also expanding its veterans program and is seeking individuals who have served to volunteer. A person does not need to be retired from the military to be considered for the volunteer position.
Those who are interested in volunteering can submit an application form online at: emmanuelhospice.org/volunteer. Individuals may contact Volunteer Coordinator Jackie Chandler for more information at jchandler@emmanuelhospice.org.