Emmanuel Hospice has been awarded a photojournalism grant valued at $35,000 by digital fundraising platform Funraise to capture patient stories and the unparalleled compassion of employees.
Emmanuel Hospice applied and received the grant near the end of 2018, chosen from several hundred applications due to its extraordinary care and devotion to their patients and outlook on the end-of-life journey.
Emmanuel’s application read in part: “Caring for the dying is not a glamorous job. In fact, it can be messy, emotionally draining, and exhausting. But it can also be joyful. It can be funny. And it can certainly be rewarding. That’s what we would love to have captured through professional images. To share the full experience of the dying with our community, and beyond. To show people that this work, while it is difficult, is also deeply profound.”
The grant will engage California photographer and videographer Alexander Pavone for one week, including his travel and lodging. Pavone will spend the week at Emmanuel Hospice in the late summer, documenting patient stories and employees’ dedication to upholding patient dignity in end-of-life care to be used for Emmanuel’s website, social media and promotional materials.
“We are really looking forward to seeing Alex’s work and how he sees our work through the lens,” said Katie Joseph, director of development at Emmanuel Hospice. “Our goal is to offer a glimpse into the reality of dying, which we believe is foundational in helping our society embrace death and live well.”
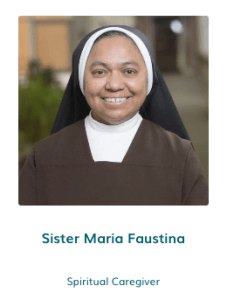
As noted in its mission statement, Emmanuel Hospice strives to provide exemplary spiritual and physical care and creating a peaceful experience for the dying. Pavone’s videos will not only provide those researching end-of-life care for their loved ones’ peace of mind, but also demonstrate the deep faith, passion and dedication at the root of all care services at Emmanuel.
Known for working with nonprofits, Funraise chose to allot a portion of its own marketing budget into several grants for capacity building, staff training and more.